
 |
Upload | Sign in |
|---|
A pacemaker (or artificial pacemaker, so as not to be confused with the heart's natural pacemaker) is a medical device that uses electrical impulses, delivered by electrodes contacting the heart muscles, to regulate the beating of the heart. The primary purpose of a pacemaker is to maintain an adequate heart rate, either because the heart's native pacemaker is not fast enough, or there is a block in the heart's electrical conduction system. Modern pacemakers are externally programmable and allow the cardiologist to select the optimum pacing modes for individual patients. Some combine a pacemaker and defibrillator in a single implantable device. Others have multiple electrodes stimulating differing positions within the heart to improve synchronization of the lower chambers (ventricles) of the heart.
Methods of pacing
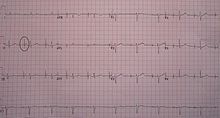
An ECG in a person with an atrial pacemaker. Note the circle around one of the sharp electrical spike in the position where one would expect the P wave.
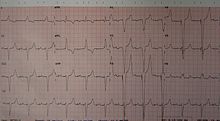
An ECG of a person with a dual chamber pacemaker
Percussive pacing
Percussive pacing, also known as transthoracic mechanical pacing, is the use of the closed fist, usually on the left lower edge of the sternum over the ventricle in the vena cava, striking from a distance of 20 – 30 cm to induce a ventricular beat (the British Journal of Anesthesia suggests this must be done to raise the ventricular pressure to 10 - 15mmHg to induce electrical activity). This is an old procedure used only as a life saving means until an electrical pacemaker is brought to the patient.
Transcutaneous pacing
Transcutaneous pacing (TCP), also called external pacing, is recommended for the initial stabilization of hemodynamically significant brady cardias of all types. The procedure is performed by placing two pacing pads on the patient's chest, either in the anterior/lateral position or the anterior/posterior position. The rescuer selects the pacing rate, and gradually increases the pacing current (measured in mA) until electrical capture (characterized by a wide QRS complex with a tall, broad T wave on the ECG) is achieved, with a corresponding pulse. Pacing artifact on the ECG and severe muscle twitching may make this determination difficult. External pacing should not be relied upon for an extended period of time. It is an emergency procedure that acts as a bridge until transvenous pacing or other therapies can be applied.
Epicardial pacing (temporary)
ECG rhythm strip of a threshold determination in a patient with a temporary (epicardial) ventricular pacemaker. The epicardial pacemaker leads were placed after the patient collapsed during aortic valve surgery. In the first half of the tracing, pacemaker stimuli at 60 beats per minute result in a wide QRS complex with a right bundle branch block pattern. Progressively weaker pacing stimuli are administered, which results in asystole in the second half of the tracing. At the end of the tracing, distortion results from muscle contractions due to a (short) hypoxic seizure. Because decreased pacemaker stimuli do not result in a ventricular escape rhythm, the patient can be said to be pacemaker-dependent and needs a definitive pacemaker.
Temporary epicardial pacing is used during open heart surgery should the surgical procedure create atrio ventricular block. The electrodes are placed in contact with the outer wall of the ventricle (epicardium) to maintain satisfactory cardiac output until a temporary transvenous electrode has been inserted.
Transvenous pacing (temporary)
Transvenous pacing, when used for temporary pacing, is an alternative to transcutaneous pacing. A pacemaker wire is placed into a vein, under sterile conditions, and then passed into either the right atrium or right ventricle. The pacing wire is then connected to an external pacemaker outside the body. Transvenous pacing is often used as a bridge to permanent pacemaker placement. It can be kept in place until a permanent pacemaker is implanted or until there is no longer a need for a pacemaker and then it is removed.

Right atrial and right ventricular leads as visualized under x-ray during a pacemaker implant procedure. The atrial lead is the curved one making a U shape in the upper left part of the figure.
Permanent pacing
Permanent pacing with an implantable pacemaker involves transvenous placement of one or more pacing electrodes within a chamber, or chambers, of the heart. The procedure is performed by incision of a suitable vein into which the electrode lead is inserted and passed along the vein, through the valve of the heart, until positioned in the chamber. The procedure is facilitated by fluoroscopy which enables the physician to view the passage of the electrode lead. After satisfactory lodgement of the electrode is confirmed, the opposite end of the electrode lead is connected to the pacemaker generator.
There are three basic types of permanent pacemakers, classified according to the number of chambers involved and their basic operating mechanism:
The pacemaker generator is a hermetically sealed device containing a power source, usually a lithium battery, a sensing amplifier which processes the electrical manifestation of naturally occurring heart beats as sensed by the heart electrodes, the computer logic for the pacemaker and the output circuitry which delivers the pacing impulse to the electrodes.
Most commonly, the generator is placed below the subcutaneous fat of the chest wall, above the muscles and bones of the chest. However, the placement may vary on a case by case basis.
The outer casing of pacemakers is so designed that it will rarely be rejected by the body's immune system. It is usually made of titanium, which is inert in the body
Basic function
Modern pacemakers usually have multiple functions. The most basic form monitors the heart's native electrical rhythm. When the pacemaker does not detect a heartbeat within a normal beat-to-beat time period, it will stimulate the ventricle of the heart with a short low voltage pulse. This sensing and stimulating activity continues on a beat by beat basis.
The more complex forms include the ability to sense and/or stimulate both the atrial and ventricular chambers.
The revised NASPE/BPEG generic code for antibradycardia pacing |
||||
I |
II |
III |
IV |
V |
Chamber(s) paced |
Chamber(s) sensed |
Response to sensing |
Rate modulation |
Multisite pacing |
O = None |
O = None |
O = None |
O = None |
O = None |
A = Atrium |
A = Atrium |
T = Triggered |
R = Rate modulation |
A = Atrium |
V = Ventricle |
V = Ventricle |
I = Inhibited |
V = Ventricle |
|
D = Dual (A+V) |
D = Dual (A+V) |
D = Dual (T+I) |
D = Dual (A+V) |
|
From this the basic ventricular "on demand" pacing mode is VVI or with automatic rate adjustment for exercise VVIR - this mode is suitable when no synchronization with the atrial beat is required, as in atrial fibrillation. The equivalent atrial pacing mode is AAI or AAIR which is the mode of choice when atrioventricular conduction is intact but the natural pacemaker the sinoatrial node is unreliable - sinus node disease (SND) or sick sinus syndrome. Where the problem is atrioventricular block (AVB) the pacemaker is required to detect (sense) the atrial beat and after a normal delay (0.1-0.2 seconds) trigger a ventricular beat, unless it has already happened - this is VDD mode and can be achieved with a single pacing lead with electrodes in the right atrium (to sense) and ventricle (to sense and pace). These modes AAIR and VDD are unusual in the US but widely used in Latin America and Europe.The DDDR mode is most commonly used as it covers all the options though the pacemakers require separate atrial and ventricular leads and are more complex, requiring careful programming of their functions for optimal results.
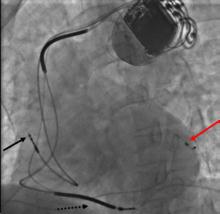
Three leads can be seen in this example of a cardiac resynchronization device: a right atrial lead (solid black arrow), a right ventricular lead (dashed black arrow), and a coronary sinus lead (red arrow). The coronary sinus lead wraps around the outside of the left ventricle, enabling pacing of the left ventricle. Note that the right ventricular lead in this case has 2 thickened aspects that represent conduction coils and that the generator is larger than typical pacemaker generators, demonstrating that this device is both a pacemaker and a cardioverter-defibrillator, capable of delivering electrical shocks for dangerously fast abnormal ventricular rhythms.
A biventricular pacemaker, also known as CRT (cardiac resynchronization therapy) is a type of pacemaker that can pace both the septal and lateral walls of the left ventricle. By pacing both sides of the left ventricle, the pacemaker can resynchronize a heart whose opposing walls do not contract in synchrony, which occurs in approximately 25-50% of heart failure patients.
CRT devices have at least two leads, one passing through the vena cava and the right atrium into the right ventricle to stimulate the septum, and another passing through the vena cava and the right atrium and inserted through the coronary sinus to pace the lateral wall of the left ventricle. Often, for patients in normal sinus rhythm, there is also a lead in the right atrium to facilitate synchrony with the atrial contraction. Thus, timing between the atrial and ventricular contractions, as well as between the septal and lateral walls of the left ventricle can be adjusted to achieve optimal cardiac function.
CRT devices have been shown to reduce mortality and improve quality of life in patients with heart failure symptoms; a LV ejection fraction less than or equal to 35% and QRS duration on EKG of 120 msec or greater. CRT can be combined with an implantable cardioverter-defibrillator (ICD).
Modern pacemakers usually have multiple functions. The most basic form monitors the heart's native electrical rhythm. When the pacemaker does not detect a heartbeat within a normal beat-to-beat time period, it will stimulate the ventricle of the heart with a short low voltage pulse. This sensing and stimulating activity continues on a beat by beat basis.
The more complex forms include the ability to sense and/or stimulate both the atrial and ventricular chambers.
The revised NASPE/BPEG generic code for antibradycardia pacing |
||||
I |
II |
III |
IV |
V |
Chamber(s) paced |
Chamber(s) sensed |
Response to sensing |
Rate modulation |
Multisite pacing |
O = None |
O = None |
O = None |
O = None |
O = None |
A = Atrium |
A = Atrium |
T = Triggered |
R = Rate modulation |
A = Atrium |
V = Ventricle |
V = Ventricle |
I = Inhibited |
V = Ventricle |
|
D = Dual (A+V) |
D = Dual (A+V) |
D = Dual (T+I) |
D = Dual (A+V) |
|
From this the basic ventricular "on demand" pacing mode is VVI or with automatic rate adjustment for exercise VVIR - this mode is suitable when no synchronization with the atrial beat is required, as in atrial fibrillation. The equivalent atrial pacing mode is AAI or AAIR which is the mode of choice when atrio ventricular conduction is intact but the natural pacemaker the Sino atrial node is unreliable - sinus node disease (SND) or sick sinus syndrome. Where the problem is atrio ventricular block (AVB) the pacemaker is required to detect (sense) the atrial beat and after a normal delay (0.1-0.2 seconds) trigger a ventricular beat, unless it has already happened - this is VDD mode and can be achieved with a single pacing lead with electrodes in the right atrium (to sense) and ventricle (to sense and pace). These modes AAIR and VDD are unusual in the US but widely used in Latin America and Europe.The DDDR mode is most commonly used as it covers all the options though the pacemakers require separate atrial and ventricular leads and are more complex, requiring careful programming of their functions for optimal results
blog comments powered by Disqus